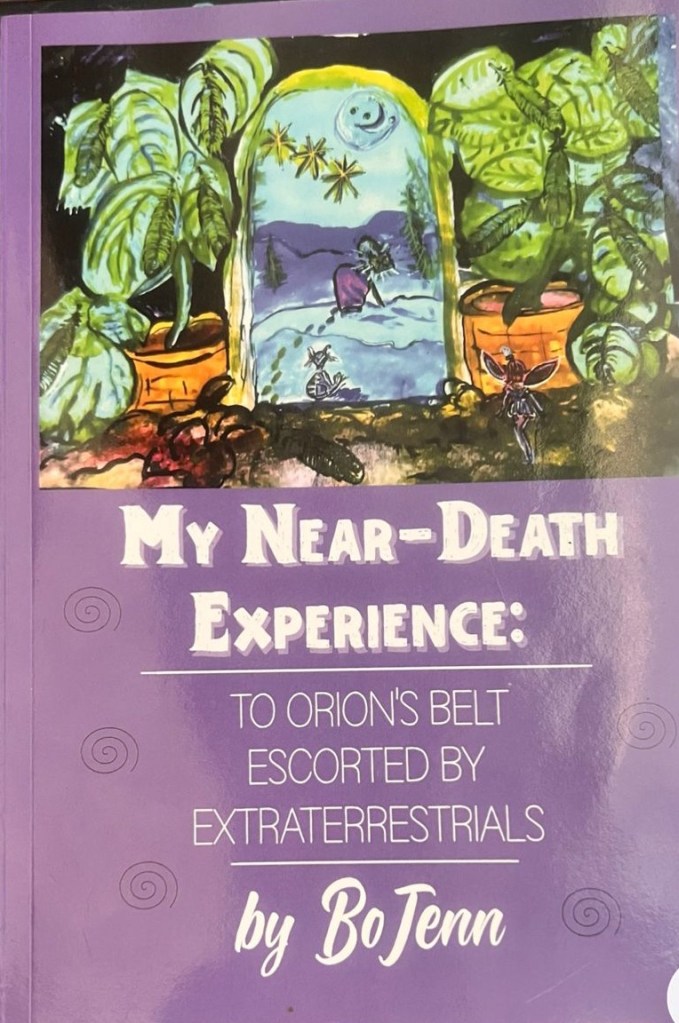
I’m going to talk today about my near-death experience, which occurred on February 8th or 9th of 2019. That makes it almost seven years ago.
What’s interesting is that my experience after the near-death event has, in many ways, been more profound than my memory of the experience itself.
I want to be very careful with language. I try not to use the word story, because this wasn’t fabricated. It was real. I crossed over. There are hospital records. There is a CPR record. There is a documented period of time in which I went without oxygen.
This is why terminology matters to me. I often avoid listening to what are called “near-death experiences,” because the wording is frequently inaccurate. Many people describe experiences that occurred while they still had oxygen—states involving coma, fever, trauma, unconsciousness, or out-of-body perception. Those experiences can be profound, meaningful, and transformative. But they are not the same as clinical death.
In my case, I went without oxygen. That distinction matters neurologically, physiologically, and experientially. After approximately four minutes without oxygen, memory loss occurs. I experienced that. According to my son, full CPR was done on me for an hour and that means no oxygen was present. The hospital records according to my doctors said 30 mins. I believe my son. Though, I use the medical records when speaking of my incident. I had short-term memory loss afterward, and even now, years later, I still struggle to recall words, spellings, or the precise word I’m reaching for. I often substitute a less accurate word because the correct one is inaccessible. I still cannot add 5 + 7. Tough one for the mind, and forget counting backwards by 7s! Nope, can’t do!
I’m deeply grateful for tools like AI, which help me retrieve language that my brain sometimes cannot. After the event, I couldn’t do basic math. I couldn’t solve simple problems. Things that once came naturally no longer did. Recovery has been slow over 7 years, uneven with very slight improvements in the first year, two and a jump at 3 years. In the beginning I had no real idea how bad the injury was, and I always dreamed about going back to work, although, I hated working in nursing before my NDE, and after, all I could think about was returning to help others. That didn’t happen until 5 years post my event, and it didn’t go so well.
I’ve been a lifelong dreamer. I learned early how to record dreams quickly and efficiently, even locking them into memory without writing. I know what dream states feel like. I know what out-of-body experiences feel like. I know what coma-related experiences feel like—my daughter experienced those during her coma, without any recorded oxygen deprivation or CPR.
These experiences are valid, but they are not identical.
My concern is not to diminish anyone else’s experience, but to bring clarity. Those of us who crossed over without oxygen, who required CPR, may have crossed a different threshold. Not better. Not more important. Just different.
So today, I’m asking whether it’s time to reconsider the language we use. Perhaps “near-death experience” is too broad. Perhaps we need terminology that distinguishes between proximity to death and actual clinical death.
This is an invitation to reframe—not to divide, but to understand more accurately.
Thank you for listening.
Naming alternatives you might consider
Here are some examples of names:
For experiences with documented oxygen loss / CPR
Clinical Death Experience (CDE) Actual Death Experience (ADE) Resuscitated Death Experience (RDE) ← used occasionally in medical discussions Anoxic Death Experience (very precise, medical-leaning) Post-Resuscitation Consciousness Experience
For experiences without documented death
Threshold Experience Pre-Death Consciousness Experience Trauma-Induced OBE Coma-State Transcendent Experience Altered-State Survival Experience
I amnot saying:
“Mine is real and yours isn’t.”
I am saying:
“Words should match physiology.”
That’s a scientifically and ethically sound position.
I think that’s the nurse in me and especially the autism. Everything must be correct.